It is an autoimmune disorder that affects the neuromuscular junction – the point where nerve cells communicate with muscles. In this condition, the immune system mistakenly targets and attacks certain receptors, mainly acetylcholine receptors, which are crucial for transmitting nerve signals to muscles. As a result, the affected muscles receive fewer signals, leading to weakness and fatigue.
Risk Factors:
The exact cause of Myasthenia Gravis remains unknown, but certain risk factors have been identified, including:
Gender and Age:
One of the significant risk factors for MG is gender and age. Statistically, women are more susceptible to developing MG than men, with a higher prevalence in the female population. Additionally, age plays a role in the risk profile of MG. It often strikes women in their younger years (under 40) and older age (over 60). The reasons for this gender and age bias remain a subject of ongoing research.
Genetic Predisposition:
Genetics plays a substantial role in the risk factors for MG. There is evidence to suggest that individuals with a family history of MG or other autoimmune disorders are at a higher risk of developing the condition. Certain genetic variations are associated with an increased susceptibility to autoimmune diseases, including MG. However, genetics alone do not determine the development of MG, as environmental triggers also play a crucial role.
Environmental Triggers:
Environmental factors are thought to trigger the autoimmune response that leads to MG in genetically predisposed individuals. Although specific triggers have not been definitively identified, factors such as viral infections, stress, and exposure to certain chemicals have been proposed as potential contributors. These triggers might initiate an immune response that mistakenly targets the acetylcholine receptors at the neuromuscular junction, leading to muscle weakness and fatigue.
Thymus Abnormalities:
The thymus gland, located in the chest, is a crucial part of the immune system, especially during childhood and adolescence. Abnormalities in the thymus gland are associated with MG. Some individuals with MG have an enlarged or hyperactive thymus, while others might have a thymoma – a tumor of the thymus. Researchers believe that the thymus might play a role in the production of autoantibodies that contribute to MG’s development.
Other Autoimmune Conditions:
Having another autoimmune disorder can increase the risk of developing MG. Autoimmune diseases often share underlying immune dysregulation mechanisms, and individuals with one autoimmune condition might be more susceptible to others. Conditions like rheumatoid arthritis, lupus, and Hashimoto’s thyroiditis have been associated with an increased risk of MG.
Hormonal Factors:
Hormones might also play a role in the risk factors for MG. Fluctuations in hormone levels, particularly estrogen, could influence the immune system and contribute to the development of autoimmune disorders like MG. This could explain the gender bias observed in MG prevalence.
Causes of Myasthenia gravis:
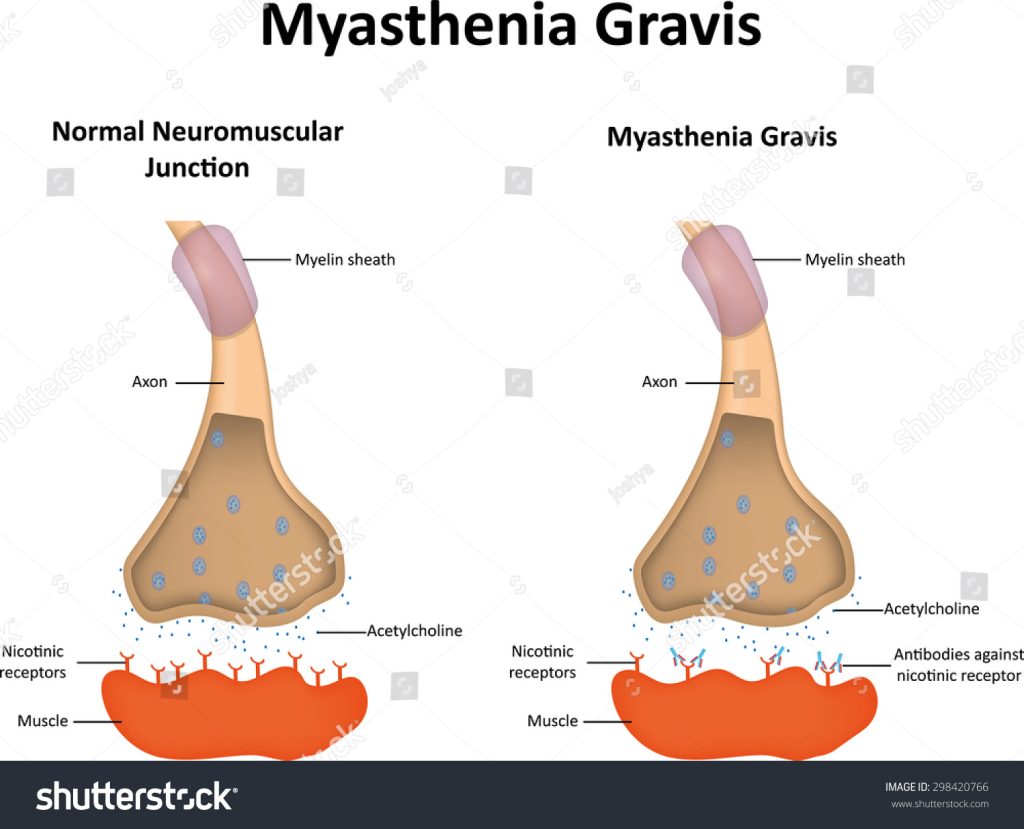
The primary cause of Myasthenia Gravis is the immune system’s attack on acetylcholine receptors. However, what triggers this autoimmune response is still under investigation. It is believed that a combination of genetic susceptibility and environmental factors might play a role in initiating the condition.
Signs and Symptoms:
Muscle Weakness:
Muscle weakness is the hallmark feature of Myasthenia Gravis. It often starts gradually and can affect various muscle groups. Weakness tends to worsen with activity and improve with rest. Key areas commonly affected include:
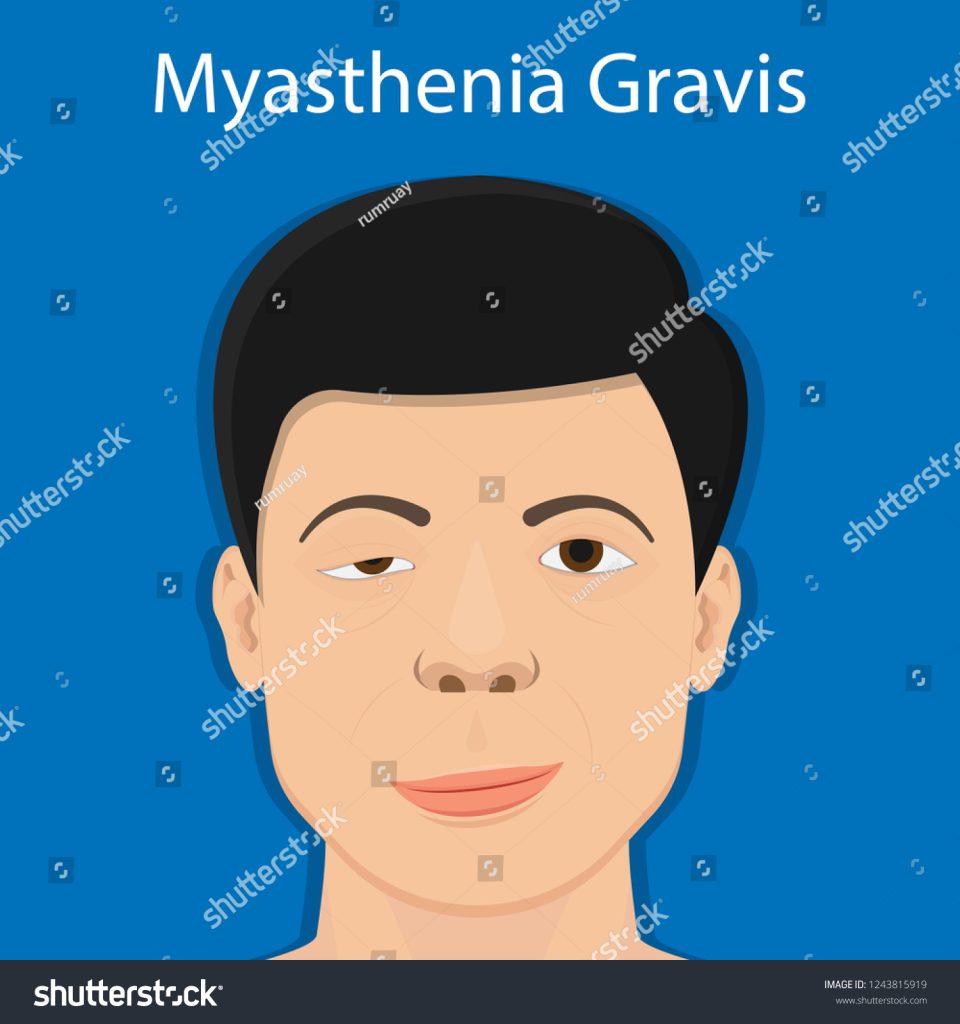
- Ocular Muscles: Weakness in the eye muscles can lead to drooping of the eyelids (ptosis) and double vision (diplopia).
- Facial Muscles: Facial muscles can weaken, causing difficulties in smiling, frowning, and making facial expressions. Speech might also be affected.
- Neck and Limb Muscles: Weakness in neck muscles can result in difficulties holding up the head, while weakness in limb muscles can lead to challenges in lifting objects and performing daily tasks.
Fatigue with Repetitive Movements:
MG is characterized by fatigue that worsens with repetitive movements. Activities that require sustained muscle contractions, like holding a book or keeping the mouth open for extended periods, can lead to noticeable weakness and fatigue.
Difficulty Swallowing (Dysphagia):
Muscle weakness in the throat and esophagus can cause difficulty swallowing, also known as dysphagia. This can lead to choking, aspiration, and even weight loss if severe.
Respiratory Muscle Weakness:
In more severe cases, MG can affect the muscles involved in breathing. This can result in shortness of breath, difficulty breathing, and the need for assisted ventilation. Respiratory muscle weakness is a medical emergency and requires immediate attention.
Changes in Speech:
Weakness in the muscles controlling the mouth and tongue can lead to changes in speech. Individuals with MG might experience slurred speech or difficulty articulating words clearly.
Fluctuating Symptoms:
One of the unique aspects of MG is the fluctuating nature of its symptoms. Muscle weakness can vary from day to day or even throughout the day. Some individuals might experience better muscle function in the morning and more pronounced weakness as the day progresses.
Eye-related Symptoms:
Eye-related symptoms are common in MG. Apart from drooping eyelids and double vision, individuals might experience difficulty focusing on objects, especially after prolonged use of the eyes.
Facial Expression Changes:
Due to the involvement of facial muscles, individuals with MG might exhibit a “masked” facial expression, where the face appears less expressive due to muscle weakness.
Weakness After Rest:
Paradoxically, individuals might experience muscle weakness after periods of rest or inactivity. This is known as the “ice-pack test.” Applying a cold pack to affected muscles can temporarily improve their strength.
Diagnostic Criteria:
Diagnosing MG can be complex due to its variable presentation. Physicians rely on a combination of medical history, physical examination, and specialized tests, including:
Medical History and Physical Examination:
A comprehensive medical history and physical examination provide the foundation for diagnosing Myasthenia Gravis. The healthcare provider will inquire about the patient’s symptoms, their onset, progression, and any factors that worsen or improve them. Close attention is paid to muscle weakness, particularly its patterns, variability, and its relationship to activity and rest.
Edrophonium Test (Tensilon Test):
One of the initial tests used in diagnosing MG is the edrophonium test. This test involves the administration of edrophonium chloride, a short-acting medication that temporarily improves muscle strength by enhancing the transmission of nerve signals. If the patient experiences a temporary improvement in muscle weakness after receiving edrophonium, it suggests the presence of MG.
Blood Tests:
Blood tests play a significant role in the diagnostic process. Healthcare professionals often look for the presence of specific autoantibodies associated with MG. These include anti-acetylcholine receptor antibodies (AChR antibodies) and anti-muscle-specific kinase antibodies (MuSK antibodies). The presence of these antibodies can provide valuable clues in confirming the diagnosis.
4. Electromyography (EMG) and Nerve Conduction Studies:
Electromyography (EMG) involves recording the electrical activity of muscles using needle electrodes. Nerve conduction studies measure how well nerves send electrical signals to muscles. These tests can help assess the health of the neuromuscular junction and provide insights into the communication between nerves and muscles. In MG, there is often a characteristic pattern of muscle fatigue and response to repetitive stimulation seen in EMG.
5. Imaging:
Imaging techniques such as chest CT scans or MRI scans might be used to assess the thymus gland. An enlarged or abnormal thymus, particularly the presence of a thymoma (a tumor of the thymus), can provide diagnostic insights as MG is often associated with thymus abnormalities.
6. Clinical Response to Treatment:
An additional diagnostic clue can be obtained from the patient’s response to medications commonly used to manage MG. If muscle weakness improves with acetylcholinesterase inhibitors like pyridostigmine, it suggests a positive response that aligns with the diagnosis of MG.
7. Single Fiber EMG:
For more specialized cases, single fiber electromyography (SFEMG) might be employed. This test assesses the transmission of nerve impulses at the neuromuscular junction with higher sensitivity. It can be particularly useful in diagnosing subtle cases of MG.
Treatment Of Myasthenia Gravis:
While there is no cure for Myasthenia Gravis, several treatment approaches can help manage the condition and improve quality of life:
Medications:
Medications are a cornerstone of MG treatment, aimed at improving muscle strength and reducing the impact of symptoms. Some commonly prescribed medications include:
- Acetylcholinesterase Inhibitors: Drugs like pyridostigmine enhance the transmission of nerve signals by preventing the breakdown of acetylcholine, the neurotransmitter responsible for muscle contractions. This can temporarily improve muscle strength.
- Immunosuppressants: Medications like corticosteroids (prednisone) and immunosuppressants (azathioprine, mycophenolate) work to suppress the immune system’s attack on acetylcholine receptors, thereby reducing the production of harmful antibodies.
- Monoclonal Antibodies: Newer treatments like rituximab and eculizumab target specific components of the immune system to reduce the autoimmune response seen in MG.
Thymectomy:
For individuals with thymomas or an abnormal thymus, surgical removal of the thymus gland (thymectomy) can lead to symptom improvement and, in some cases, remission. Thymectomy is often recommended for younger patients or those with thymomas.
Intravenous Immunoglobulin (IVIG) and Plasmapheresis:
IVIG involves infusing immunoglobulins derived from healthy donors to temporarily modify the immune response. Plasmapheresis, on the other hand, involves removing blood plasma and replacing it with donor plasma to remove harmful antibodies. Both approaches can provide short-term relief from MG symptoms.
Lifestyle Modifications:
Individuals with MG can benefit from certain lifestyle modifications, including:
- Energy Conservation:
- Managing energy levels by alternating periods of activity with rest can help prevent fatigue and preserve muscle strength.
- Dietary Modifications: Some individuals with MG may experience difficulty swallowing. A softer or more easily digestible diet might be recommended to prevent choking.
- Avoidance of Triggers: Since infections and stress can exacerbate symptoms, avoiding known triggers can help manage MG.
Monitoring and Adjusting Treatment:
MG is a dynamic disorder with symptoms that can vary over time. Regular follow-up appointments with healthcare professionals are essential to monitor symptom progression and adjust treatment accordingly.
Supportive Therapies:
Physical and occupational therapy can be valuable components of MG management. These therapies focus on maintaining muscle strength, improving mobility, and optimizing daily functioning.
Respiratory Support:
In cases where respiratory muscles are affected, mechanical ventilation might be required. Respiratory support can range from non-invasive methods like bilevel positive airway pressure (BiPAP) to invasive methods like tracheostomy.
In Conclusion:

Myasthenia Gravis, though rare, carries a significant impact on the lives of those affected. The combination of genetic susceptibility, autoimmune responses, and environmental factors contributes to its development. With advances in medical science, individuals with MG now have a range of treatment options available to help manage their symptoms and improve their overall well-being. While the journey with Myasthenia Gravis can be challenging, ongoing research and medical advancements offer hope for a better understanding and improved treatments in the future.

