Poliomyelitis, often referred to simply as polio, is a highly infectious viral disease caused by the poliovirus. It primarily affects young children and can lead to paralysis, muscle weakness, and even death in severe cases. The virus spreads primarily through the fecal-oral route, usually entering the body through contaminated water or food. It can also spread through direct contact with an infected person’s saliva or mucus.
Types of poliomyelitis:
Poliomyelitis, commonly known as polio, is caused by the poliovirus, which has three distinct serotypes: type 1, type 2, and type 3. Each serotype can cause polio, and they are collectively referred to by their numerical designations. Here are the three types of polio with their names:
Type 1 Poliovirus: Also known as “Poliovirus Type 1” or simply “Type 1,” this serotype is responsible for the majority of polio cases and historically has been the most widespread.
Type 2 Poliovirus: Similarly referred to as “Poliovirus Type 2” or “Type 2,” this serotype is less common than type 1 but has been associated with significant outbreaks. As of 2016, the type 2 component of the oral polio vaccine (OPV) has been removed due to concerns about vaccine-derived cases.
Type 3 Poliovirus: Known as “Poliovirus Type 3” or “Type 3,” this serotype is less frequently linked to polio cases compared to types 1 and 2. Like type 2, the type 3 component of the OPV was removed in 2016.
Risk Factors:
Several risk factors can increase the likelihood of exposure to the poliovirus and the development of polio. These risk factors include:
Lack of Vaccination: The most significant risk factor for polio is not being vaccinated. People who have not received the polio vaccine are at a higher risk of contracting the virus. This is particularly relevant in areas with low vaccination rates or limited access to healthcare.
Inadequate Hygiene and Sanitation: Poliovirus spreads through the fecal-oral route, often due to contaminated water and food. Poor hygiene practices, inadequate sanitation facilities, and lack of clean drinking water can contribute to the spread of the virus.
Close Contact with an Infected Person: The virus can spread through direct contact with an infected person’s saliva, mucus, or feces. Living in close quarters with someone who has the virus, such as within a household or community, can increase the risk of transmission.
Travel to High-Risk Areas: Traveling to regions where polio is still endemic or where there are outbreaks increases the risk of exposure to the virus. Travelers should ensure they are vaccinated appropriately before visiting these areas.
Weakened Immune System: Individuals with weakened immune systems, such as those with certain medical conditions or undergoing immunosuppressive treatment, may be more susceptible to contracting the virus if exposed.
Age: Polio primarily affects young children, especially those under the age of 5. Children in this age group are more likely to develop severe symptoms if infected.
Seasonal Factors: Polio transmission can vary with season. In some regions, the virus may be more active during certain times of the year, which can contribute to higher rates of transmission.
Social and Economic Factors: Poverty, overcrowding, and lack of access to clean water and sanitation facilities can create an environment conducive to the spread of poliovirus.
Causes of Polio:
Polio is caused by infection with the poliovirus, which spreads primarily through contaminated water or food, or through direct contact with an infected person’s saliva or mucus. The virus attacks the nervous system, leading to muscle weakness, paralysis, and in severe cases, even death. Vaccination is the most effective way to prevent polio.
Signs and Symptoms:
The symptoms of polio can vary widely, ranging from no noticeable symptoms to severe paralysis and even death. There are two main types of polio: non-paralytic (abortive) and paralytic.
Non-Paralytic (Abortive) Polio:
- Fever
- Sore throat
- Headache
- Nausea and vomiting
- Fatigue
- Muscle stiffness
- Pain and discomfort in muscles and joints
- Generally mild symptoms that may last a few days to a week
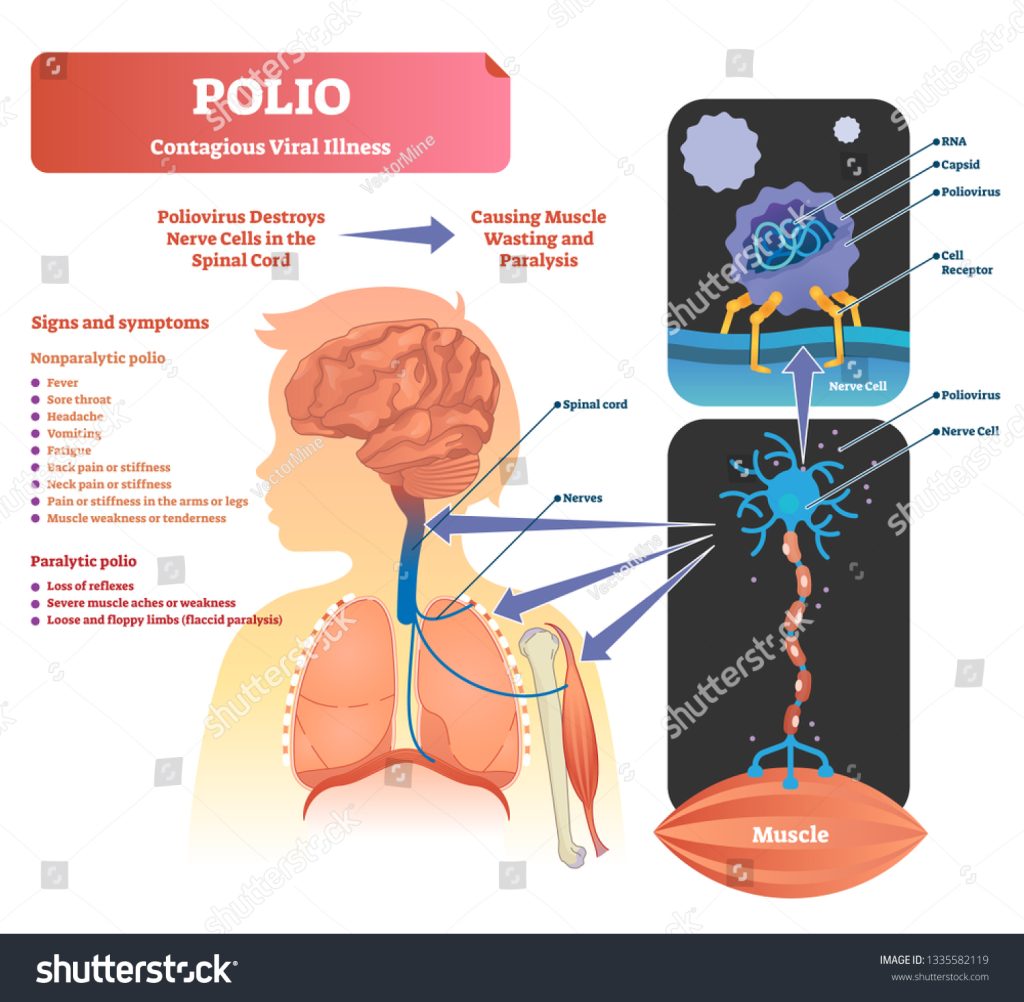
Paralytic Polio:
- Initial symptoms similar to non-paralytic polio
- Gradual onset of muscle weakness or paralysis, usually affecting one side of the body more than the other
- Severe cases can lead to difficulty breathing and require ventilator support
- Muscle pain and spasms
- Loss of reflexes
- Permanent disability if not treated promptly
In severe cases, paralysis can affect the legs, arms, and sometimes the muscles required for breathing, which can be life-threatening
It’s important to note that most polio infections (about 90-95%) result in mild or no symptoms, referred to as subclinical infections. Only a small percentage of cases progress to paralytic polio. Additionally, even after recovery from acute symptoms, some individuals may experience post-polio syndrome years later, characterized by new muscle weakness, fatigue, and pain.
Diagnostic Criteria:
The diagnosis of polio involves considering a combination of clinical symptoms, laboratory testing, and epidemiological factors. The World Health Organization (WHO) provides guidelines for the clinical diagnosis of polio, which include the following criteria:
Acute Flaccid Paralysis (AFP): The primary clinical feature of paralytic polio is the sudden onset of acute flaccid paralysis (AFP), which is characterized by rapid muscle weakness or loss of muscle tone in one or more limbs. The paralysis is usually asymmetrical.
Exclusion of Other Causes: Other potential causes of acute flaccid paralysis, such as Guillain-Barré syndrome, transverse myelitis, and viral myositis, must be carefully excluded through clinical evaluation and appropriate diagnostic tests.
Laboratory Confirmation: Laboratory testing is an essential component of the diagnostic process. Stool samples are collected from suspected cases of polio to detect the presence of the poliovirus through viral isolation or identification of viral genetic material (RNA).
Epidemiological Factors: The diagnosis also takes into account epidemiological factors such as the patient’s age, vaccination history, and whether there is ongoing poliovirus circulation in the region.
Treatment Of Poliomyelitis:

Currently, there is no specific cure for polio once a person becomes infected with the poliovirus. However, the treatment of polio primarily focuses on managing symptoms, preventing complications, and providing supportive care. The severity of the disease can vary, ranging from mild symptoms to severe paralysis. Here are the key aspects of treatment for polio:
Supportive Care: Patients with non-paralytic polio (mild cases) typically require rest, fluids, and over-the-counter pain relievers to manage symptoms like fever and muscle pain.
Physical Therapy: For individuals with paralytic polio (severe cases involving muscle weakness or paralysis), physical therapy is crucial. It helps maintain and improve muscle strength and function, prevent joint contractures, and enhance overall mobility.
Assistive Devices: Depending on the extent of paralysis, patients might need assistive devices such as braces, crutches, wheelchairs, or orthopedic appliances to support their mobility.
Respiratory Support: In cases where the virus affects the muscles responsible for breathing, mechanical ventilation or other respiratory support may be necessary to ensure adequate oxygen supply.
Pain Management: Paralytic polio can cause muscle pain and discomfort. Pain relief medications and physical therapies may be used to alleviate these symptoms.
Prevention of Secondary Infections: Patients with polio are at an increased risk of developing secondary infections due to their compromised mobility. Preventing infections is essential, and vaccinations against other diseases can help.
Long-Term Monitoring: Some individuals who recover from acute polio symptoms might experience late effects known as post-polio syndrome, which includes new muscle weakness, fatigue, and pain. Long-term monitoring and management are important for these cases.
Physical Therapy Management:
The physical therapy management of polio aims to improve mobility, function, and quality of life for individuals affected by the disease, especially those with residual muscle weakness or paralysis. Keep in mind that the specific physical therapy plan will vary based on individual needs, the extent of paralysis, and the availability of resources. Here’s a general overview of the components of physical therapy management for polio:
Assessment and Evaluation:
A thorough assessment of the patient’s medical history, current physical condition, and functional limitations is conducted.
Evaluation of muscle strength, joint range of motion, balance, gait, and overall mobility is performed.
Goal Setting:
Establish clear and realistic goals based on the patient’s abilities, needs, and aspirations. Goals may include improving walking ability, increasing independence, and reducing pain.
Muscle Strengthening:
Develop an individualized strengthening program to target weak muscles while taking care not to overwork already compromised muscles.
Strengthening exercises might involve resistance training, isometric exercises, and functional activities.
Range of Motion Exercises:
Passive and active range of motion exercises are used to maintain joint flexibility and prevent contractures.
Gentle stretching can help prevent muscle and joint stiffness.
Gait Training:
Focus on teaching or retraining proper walking patterns and techniques.
Assistive devices like crutches, walkers, or orthotics may be introduced to improve stability and support.
Balance and Coordination:
Balance training exercises help improve stability and prevent falls.
Coordination exercises can enhance overall movement control.
Functional Training:
Incorporate activities that simulate daily tasks and challenges to enhance functional independence.
Functional training might involve getting in and out of bed, getting dressed, and other routine activities.
Pain Management:
Address pain or discomfort associated with muscle weakness or strain through appropriate exercises and techniques.
Modalities like heat, ice, or transcutaneous electrical nerve stimulation (TENS) might be used.
Breathing Exercises:
If respiratory muscles are affected, respiratory exercises may be prescribed to improve breathing capacity and function.
Energy Conservation:
Teach strategies to manage fatigue and conserve energy during daily activities.
Patient Education:
Educate patients and their families about proper body mechanics, safe mobility techniques, and strategies for preventing complications.
Long-Term Management:
Develop a plan for ongoing monitoring and adjustments to the physical therapy program as needed, especially considering potential late effects like post-polio syndrome.
Psychosocial Support:
Provide emotional support and encouragement to help patients cope with the challenges of living with polio-related disabilities.
In Conclusion:

Poliomyelitis, commonly known as polio, is a viral disease caused by the poliovirus. It primarily affects the nervous system, leading to varying degrees of muscle weakness and paralysis, with severe cases posing a risk to breathing and mobility. Thanks to widespread vaccination efforts, polio has been significantly reduced globally. However, challenges remain in eradicating the virus entirely, particularly in regions with limited healthcare access. Comprehensive vaccination, public health surveillance, and appropriate medical care are crucial in the ongoing endeavor to eliminate polio and ensure a polio-free world.

